Lung Test Biography
(Source google.com)
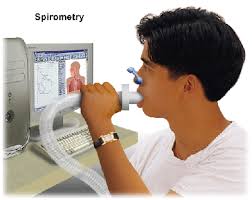
Spirometry (meaning the measuring
of breath) is the most common of the pulmonary function tests (PFTs), measuring
lung function, specifically the amount (volume) and/or speed (flow) of air that
can be inhaled and exhaled. Spirometry is an important tool used for generating
pneumotachographs, which are helpful in assessing conditions such asasthma,
pulmonary fibrosis, cystic fibrosis, and COPD. The basic forced volume vital
capacity test varies slightly depending on the equipment used.
Generally, the patient is asked
to take the deepest breath they can, and then exhale into the sensor as hard as
possible, for as long as possible, preferably at least 6 seconds. It is
sometimes directly followed by a rapid inhalation (inspiration), in particular
when assessing possible upper airway obstruction. Sometimes, the test will be
preceded by a period of quiet breathing in and out from the sensor (tidal
volume), or the rapid breath in (forced inspiratory part) will come before the
forced exhalation.
During the test, soft nose clips
may be used to prevent air escaping through the nose. Filter mouthpieces may be
used to prevent the spread of microorganisms. The maneuver is highly dependent
on patient cooperation and effort, and is normally repeated at least three times
to ensure reproducibility. Since results are dependent on patient cooperation,
FVC can only be underestimated, never overestimated. Due to the patient
cooperation required, spirometry can only be used on children old enough to
comprehend and follow the instructions given (6 years old or more), and only on
patients who are able to understand and follow instructions — thus, this test
is not suitable for patients who are unconscious, heavily sedated, or have
limitations that would interfere with vigorous respiratory efforts. Other types
of lung function tests are available for infants and unconscious persons. Another major limitation is the
fact that many intermittent or mild asthmatics have normal spirometry between
acute exacerbation, limiting spirometry's usefulness as a diagnostic. It is
more useful as a monitoring tool: a sudden decrease in FEV1 or other spirometric
measure in the same patient can signal worsening control, even if the raw value
is still normal. Patients are encouraged to record their personal best
measures. Spirometry can also be part of a
bronchial challenge test, used to determine bronchialhyperresponsiveness to
either rigorous exercise, inhalation of cold/dry air, or with a pharmaceutical
agent such as methacholine or histamine.
Sometimes, to assess the
reversibility of a particular condition, a bronchodilator is administered
before performing another round of tests for comparison. This is commonly
referred to as a reversibility test, or a post bronchodilator test (Post BD),
and is an important part in diagnosing asthma versus COPD. Other complementary
lung functions tests include plethysmography and nitrogen washout. The most common parameters
measured in spirometry are Vital capacity (VC), Forced vital capacity (FVC),
Forced expiratory volume at timed intervals of 0.5, 1.0 (FEV1), 2.0, and
3.0 seconds, forced expiratory flow and maximal voluntary
ventilation (MVV), also known as Maximum breathing capacity. Other tests may be
performed in certain situations.
Results are usually given in both
raw data (litres, litres per second) and percent predicted—the test result as a
percent of the "predicted values" for the patients of similar
characteristics (height, age, sex, and sometimes race and weight). The
interpretation of the results can vary depending on the physician and the
source of the predicted values. Generally speaking, results nearest to 100%
predicted are the most normal, and results over 80% are often considered
normal. Multiple publications of predicted values have been published and may
be calculated online based on age, sex, weight and ethnicity. However, review
by a doctor is necessary for accurate diagnosis of any individual situation. A
bronchodilator is also given in certain circumstances and a pre/post graph
comparison is done to assess the effectiveness of the bronchodilator. See the
example printout. Functional residual capacity (FRC) cannot be measured via
spirometry, but it can be measured with a plethysmograph or dilution tests (for
example, helium dilution test). is the ratio of .
In healthy adults this should be approximately 75–80%. In obstructive diseases
(asthma, COPD, chronic bronchitis, emphysema) is diminished because of
increased airway resistance to expiratory flow; the FVC may be decreased as
well, due to the premature closure of airway in expiration, just not in the
same proportion as (for instance, both and FVC are reduced, but the
former is more affected because of the increased airway resistance). This
generates a reduced value (<80%, often ~45%). In restrictive diseases (such
as pulmonary fibrosis) the and FVC are both reduced proportionally and the
value may be normal or even increased as a result of decreased lung compliance.
A derived value of is predicted, which is defined as of the patient divided by the average in the population for any person of similar age, sex and body
composition. Forced expiratory flow is
the flow (or speed) of air coming out of the lung during the middle portion of
a forced expiration. It can be given at discrete times, generally defined by
what fraction remains of the forced vital capacity . The usual intervals, or 25% and 50% of . It can
also be given as a mean of the flow during an interval, also generally
delimited by when specific fractions remain of , .
Average ranges in the healthy population depend mainly on sex and age, with
FEF25–75% shown in diagram at left. Values ranging from 50-60% and up to 130%
of the average are considered normal. Predicted normal values for FEF can be
calculated online and depend on age, sex, height, mass and ethnicity as well as
the research study that they are based on. stands for maximal
(mid-)expiratory flow and is the peak of expiratory flow as taken from the
flow-volume curve and measured in liters per second. It should theoretically be
identical to peak expiratory flow , which is, however, generally measured
by a peak flow meter and given in liters per minute. Recent research suggests that may be a more sensitive parameter than in the
detection of obstructive small airway disease. However, in the absence of
concomitant changes in the standard markers, discrepancies in mid-range
expiratory flow may not be specific enough to be useful, and current practice
guidelines recommend continuing to use, and as indicators of
obstructive disease.












No comments:
Post a Comment